Chi siamo
Fighting the war on Malaria

Malaria kills 780,000 people every year – most of them in Africa. Its effects have trapped millions in an endless cycle of poverty, but thanks to a massive international push to control the disease, it may finally be losing its grip. Could this be the beginning of the end for malaria?
The statistics may appear bleak: In 2012, every 45 seconds a child dies of malaria and over 780,000 people in total die from the disease every year. Yet compared with three years before – when it was estimated that a child died of malaria every 30 seconds, with nearly one million total fatalities worldwide – those figures offer some hope.
The truth is, cases of malaria are falling – thanks to what is arguably the most organized collective campaign against the disease the world has ever seen. Since the late 1990s, efforts to reduce the malaria burden have been gathering pace, with public health organizations, aid agencies, governments and private enterprises combining their resources. This is organized through a set of new inter-agency partnerships and initiatives that include the Global Fund to Fight AIDS, Tuberculosis and Malaria, as well as the President’s Malaria Initiative in the United States, and Roll Back Malaria.
The collective effort is focused on achieving U.N. Millennium Development Goals (MDGs) – one of which is to halt and begin to reverse the incidence of malaria and other major diseases by 2015. The Roll Back Malaria partnership has taken this still further with a goal of near-zero deaths from malaria by 2015 – with the ultimate aim of eradicating malaria altogether.

Pregnant women and children are the most vulnerable to malaria. It contributes to the deaths of an estimated 10,000 pregnant women and up to 200,000 infants each year in Africa alone.
Unlike other deadly diseases, malaria is both curable and preventable. Research has also demonstrated that the economic and social effects of malaria are devastating. Malaria keeps children away from school and adults from work; it pulls families into poverty and keeps them there.
Predictably, its greatest impact is on the world’s poorest – those who simply cannot afford treatment or who have limited access to healthcare. Overall, malaria causes an average loss of 1.3% of annual economic growth in countries with high transmission rates. Tackle malaria and you go a long way to tackling endemic poverty in many countries.
This isn’t the first time the world has tried to stop malaria. In 1955, the World Health Organization (WHO) submitted an ambitious proposal for the eradication of malaria worldwide.
Some countries managed it; others were less successful, with initial reductions followed by sharp increases once efforts ceased.
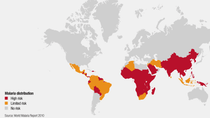
Climate apparently made the difference between success and failure: In temperate countries where malaria is a seasonal disease, eradication was possible. Not so for countries where malaria is rife all year round. The climate factor at least partly explains why it is sub-Saharan Africa that bears the brunt of the malaria burden: Around 90% of all malaria cases occur in Africa.
Critics are quick to question why, if eradication didn’t work in the 1950s, it will work now. But much has changed: Advances in public health knowledge, treatment and technology have allowed the development of coherent and effective malaria control strategies, as set out by WHO and in the Global Malaria Action Plan.
20%
Malaria causes 20% of all childhood deaths in Africa.
40%
Malaria accounts for approximately 40% of public health spending in sub-Saharan Africa, 20% to 50% of inpatient admissions and 50% of outpatient admissions.
85%
85% of all malaria deaths occur in children under the age of five.
4.2 million
It is estimated that 4.2 million lives would be saved by full coverage of malaria control measures – i.e. use of nets, spraying, diagnosis, drugs – by 2015 in the 20 most at-risk African countries.
Getting results
The last decade has also seen a series of innovations that make fulfillment of the 2015 goal achievable. The first of these is the long-lasting insecticide-treated net (LLIN). Lasting at least three years, these nets have been shown to lower transmission by 90%, malaria incidence by 50%, and child mortality by 15%. Over the last few years, there has been a massive international push to deliver these nets: WHO has reported that 289 million nets were delivered to sub-Saharan Africa between 2008 and 2010. That is enough to cover 76% of the population at risk.
Indoor residual spraying (IRS) – where walls are sprayed with insecticide – has also been shown to reduce transmission, and WHO recommends it be used in tandem with LLINs. Here again, distribution has been impressive, with 73 million people in Africa protected from malaria with IRS programs, up from 13 million in 2005.
The last decade has also seen the arrival of larvicides, a new generation of anti-malarial drugs, and Rapid Diagnostic Tests, which enable earlier diagnosis and more accurate treatment.
The distribution of these technologies together with better case management and education has delivered positive results. Eleven African countries have reported a decrease of at least 50% in malaria cases between 2000 and 2009. By 2009, the annual number of malaria deaths had fallen by 20% in comparison with the beginning of the millennium. In 2010, Morocco and Turkmenistan were certified by the Director-General of WHO as having eliminated malaria.

A challenging future
In other words, the push to reduce malaria cases is working – but there are still plenty of challenges ahead. Of particular concern is the distribution of nets. Roll Back Malaria estimates that 100 million LLINs must be financed and distributed globally every year, to sustain coverage and replace worn-out nets. But with distribution bottlenecks still an issue in some countries, this is proving difficult to achieve – as is the organization of IRS.
A resurgence in cases has been observed in parts of at least three African countries: Rwanda, Sao Tome and Principe, and Zambia. The reasons for this are uncertain, but one possible cause is a relaxation of control efforts; in Sao Tome and Principe, the resurgences followed a year in which IRS wasn’t deployed, for example.

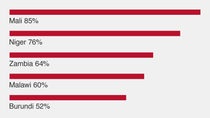
Percentage of households owning at least one insecticide-treated net, 2010
(Source: UNICEF global malaria databases 2011)
There is also the ever-looming threat of resistance to commonly-used insecticides, and drug resistance. In Cambodia, artemisinin-based drugs – currently hoped to be the most effective form of malaria treatment – are now taking longer to take effect. It’s unclear as to why, but it was in the same region that resistance developed to the older antimalarial drugs chloroquine and mefloquine.
These challenges cannot be addressed unless the global community sustains its investment and interest in the 2015 goal.
There is now growing concern that the campaign may fall victim to its own success: As the burden of disease falls away, political resolve could weaken and financial commitments diminish. Given the current global recession there is a genuine fear that malaria control could move down the list of development priorities. And yet there is hope: In 2012 the U.K. government announced it would be increasing its investment in the malaria campaign, for example. If the global community manages to sustain momentum, the eradication of malaria could be a distinct possibility.





